References:
1. Kessler, R.C., Berglund, P., Delmer, O., Jin, R., Merikangas, K.R., & Walters, E.E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6): 593-602.
2. Tanielian, T. & Jaycox, L. (Eds.). (2008). Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation.
3. Angelucci F, Ricci V, Gelfo F, et al. BDNF serum levels in subjects developing or not post-traumatic stress disorder after trauma exposure. Brain Cogn. 2014;84(1):118‐122. doi:10.1016/j.bandc.2013.11.012
4. Huang YJ et al. New Treatment Strategies of Depression: Based on Mechanisms Related to Neuroplasticity. Neural Plast. 2017; 2017:4605971.
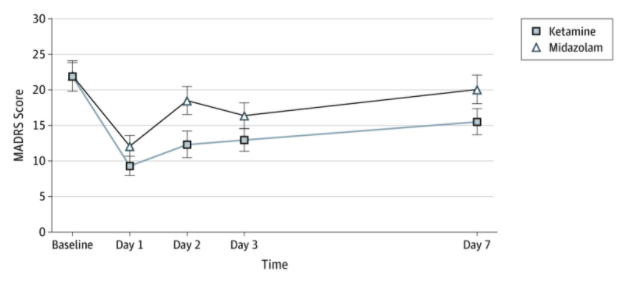
5. Feder A, Parides MK, Murrough JW, et al. Efficacy of Intravenous Ketamine for Treatment of Chronic Posttraumatic Stress Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2014;71(6):681–688. doi:10.1001/jamapsychiatry.2014.62
6. Jennifer Dore et al. Ketamine Assisted Psychotherapy (KAP): Patient Demographics, Clinical Data and Outcomes in Three Large Practices Administering Ketamine with Psychotherapy, Journal of Psychoactive Drugs, 51:2, 189-198, DOI: 10.1080/02791072.2019.1587556.